Multiple myeloma is an incurable bone marrow cancer that kills over 100,000 people every year. Known for its quick and deadly spread, this disease is one of the most challenging to address. As these cancer cells move through different parts of the body, they mutate, outpacing possible treatments. People diagnosed with severe multiple myeloma that is resistant to chemotherapy typically survive for only three to six months. Innovative therapies are desperately needed to prevent the spread of this disease and provide a fighting chance for those who suffer from it.
Michael Mitchell, J. Peter and Geri Skirkanich Assistant Professor of Innovation in Bioengineering (BE), and Christian Figueroa-Espada, doctoral student in BE at the University of Pennsylvania School of Engineering and Applied Science, created an RNA nanoparticle therapy that makes it impossible for multiple myeloma to move and mutate. The treatment, described in their study published in PNAS, turns off a cancer-attracting function in blood vessels, disabling the pathways through which multiple myeloma cells travel.
By shutting down this “chemical GPS” that induces the migration of cancer cells, the team’s therapy stops the spread of multiple myeloma, helping to eliminate it altogether.
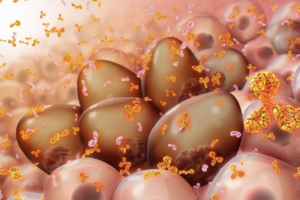
Endothelial cells, those that line blood vessels, produce a protein we need to survive. This protein, CyPA, is responsible for folding and transporting other proteins. It also activates T-cell responses when we get sick.
However, when multiple myeloma is present, endothelial cells overexpress CyPA and secrete it into the blood vessels where its functions become malignant. Here, CyPA is a chemo-attractant, meaning it pulls multiple myeloma cells from the bone marrow into the blood vessels where they travel quickly to other bones in the body.
“To stop the spread, we aimed to turn off this function of CyPA using RNA therapy, targeting the microenvironment of the cancer instead of the cancer cell itself,” says Mitchell. “But getting nucleic acids into the marrow was challenging due to the complex biological barriers.”
To get the RNA into the hard-to-reach bone marrow, the team needed to redesign the traditional delivery vehicle for the lipid nanoparticle.
“We designed a new hybrid nanoparticle that could deliver small interfering RNA (siRNA) to endothelial cells,” says Figueroa-Espada. “The siRNA stops cells from producing CyPA. When tested in vitro, the therapy prevented the spread of cancer cells. When tested in mice, both alone and in combination with chemotherapies, our therapy was able to decrease the size of tumors, extend survival rates and decrease the cancer’s resistance to chemotherapy.”
“This work can help improve current treatments for multiple myeloma as well as other cancers that spread through the blood vessels,” adds Mitchell. “Using our platform for targeted nanoparticle development, we are looking forward to investigating other cancers and diseases where CyPA is overexpressed.”
By creating a roadblock in cancer’s commute through the body, the Penn Engineering team is removing a longstanding barrier in the treatment of multiple myeloma, providing real hope for people diagnosed with this disease.
In future work, the team plans to investigate silencing additional functions in the microenvironments of cancers to better overcome drug resistance, cancer initiation, and metastasis. They are currently working with Ruben Carrasco, Professor of Pathology at the Dana-Farber Cancer Institute and co-corresponding author of this study, to identify potential targets for this kind of therapy. Once RNA nanoparticle therapy is proven safe in larger animals, this proof-of-concept study can move forward to clinical trials.
