Penn Engineers Test Drug Transfer Using Placenta-on-a-Chip
Researchers at the University of Pennsylvania’s School of Engineering and Applied Science have demonstrated the feasibility of their “organ-on-a-chip” platform in studying how drugs are transported across the human placental barrier.
Some maternally-administered medications can enter the fetal bloodstream, but how the placenta determines which molecules can get through is still poorly understood. The ways of testing this process are limited. Animal models don’t capture important details of human physiology, most in vivo research can’t be ethically performed, and placentas donated after birth are only viable for a few hours, making it difficult to properly conduct complicated transport experiments.
A small number of drugs have been tested via this “ex vivo placental perfusion” method, however. By comparing the results of transport experiments conducted on their placenta-on-a-chip, the Penn team demonstrated their benchtop system could be an effective stand-in for a living organ in such research.
The study was led by Dan Huh, Wilf Family Term Assistant Professor in Bioengineering in Penn’s School of Engineering and Applied Science, and Cassidy Blundell, a graduate student in the Huh lab. Other lab members, Yoon-Suk Yi, Lin Ma, Emily Tess, Megan Farrell and Andrei Georgescu, contributed to the study. They collaborated with Lauren M. Aleksunes, an associate professor in Rutgers University’s Ernest Mario School of Pharmacy.
It was featured on the cover of the journal Advanced Healthcare Materials.
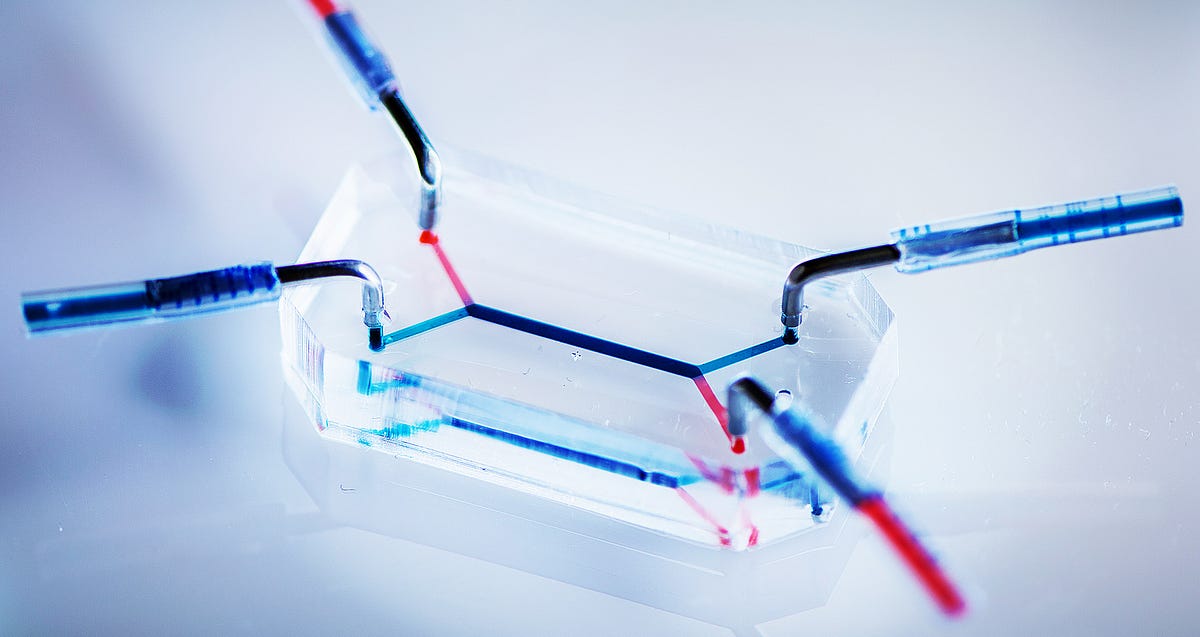
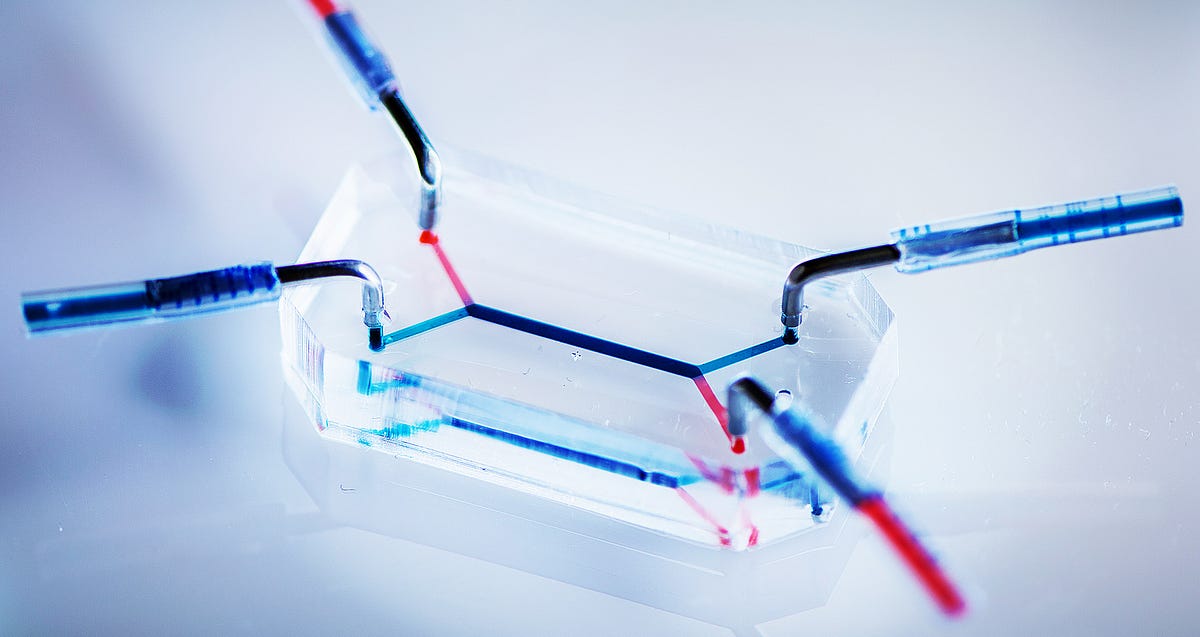
The Penn team’s placenta-on-a-chip is a small block of silicone that houses two microfluidic channels separated by a porous membrane. The researchers grow human trophoblast cells on one side of the membrane and endothelial cells on the other. The layers of those two cell types mimic the placental barrier, which determines what passes from the maternal to the fetal circulatory systems.
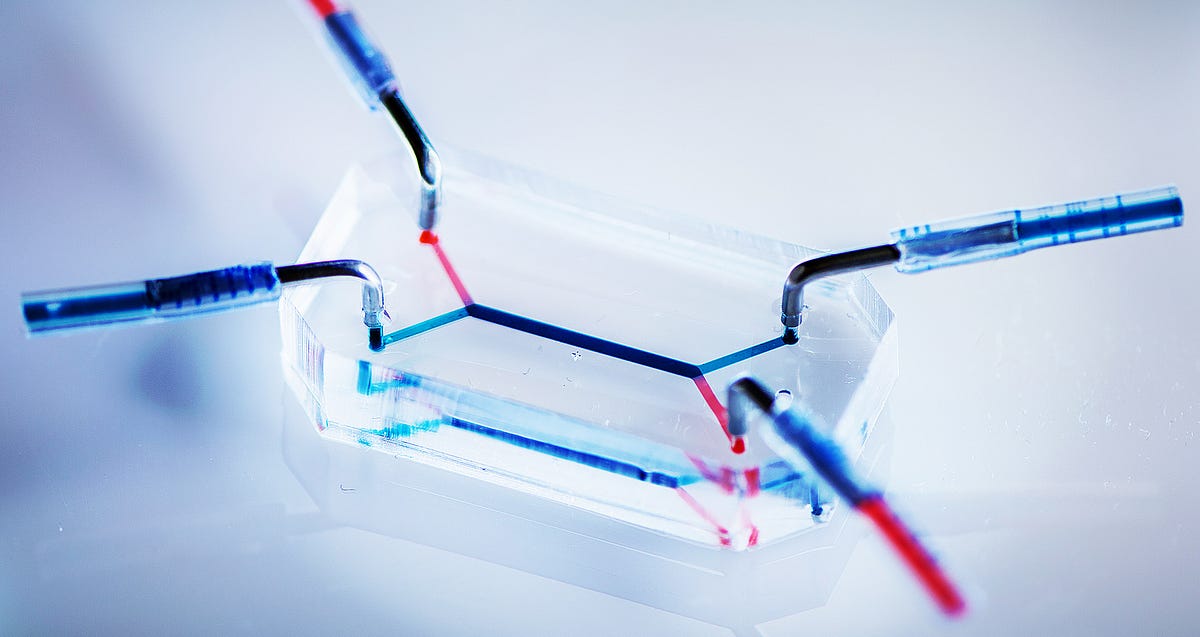
By adding different molecules to the blood-like fluid flowing through the “maternal” microfluidic channel, the researchers can measure the rate at which they transfer to the “fetal” channel and how much they accumulate in the barrier itself.
The ability to test this process on human placentas is in high demand. Pregnant women are excluded from clinical drug trials, and animal models have severe limitations. Those limitations were tragically demonstrated in the case of thalidomide, where a morning sickness drug able to transport across the human placental barrier led to tens of thousands of birth defects and deaths.
Current state-of-the-art transport experiments are conducted on donated human placental tissue, but hooking up a living organ to the testing apparatus is a messy, finicky proposition.
“Ex vivo placental perfusion is a great method,” Huh said, “but it has a pretty high failure rate, and the experimental set-up is complicated: it’s prone to leaks and needs a high level of expertise. Most pharmaceutical companies are not going to be able to test their drugs using this method.”
To validate their placenta-on-a-chip as a testing platform, Huh and his colleagues compared the transport of two drugs that have been studied via ex vivo placental perfusion: heparin, an anticoagulant, and glyburide, used in the treatment of diabetes.
Heparin is understood to be too large a molecule to pass through the placental barrier, and the team’s placenta-on-a-chip also bore out that result. Glyburide has been found to be carried by specialized efflux transporters expressed by the placental tissue that limit fetal exposure to maternally administered drug molecules. The placenta-on-a-chip was able to emulate this protective mechanism.
“We’re getting close,” Huh said. “This study has given us confidence that the placenta-on-a-chip has tremendous potential as a screening platform to assess and predict drug transport in the human placenta.”
Further research and validation studies will be necessary before the placenta-on-a-chip sufficiently replicates its in vivo counterpart for the purposes of clinical testing.
“For example, the fluorescent marker we use changes the size and other characteristics of the drug, which has an effect on transport,” Blundell said. “In future studies, we will work with our collaborator, Lauren Aleksunes, and her lab to test drugs without this fluorescent tag.”
Beyond pharmaceuticals, the Penn team’s placenta-on-a-chip would be useful for better understanding the health impacts of a variety of things that could potentially cross into the fetal bloodstream.
“There’s also the potential to use our system to evaluate the transfer of substances other than drugs. We can test herbal supplements, vitamins, and additional products that a woman might take during her pregnancy,” Blundell said.
The research was supported by the March of Dimes Prematurity Research Center at the University of Pennsylvania, and the National Institutes of Health through the NIH Director’s New Innovator Award 1DP2HL127720–01 and grants R01ES020522 and P30ES005022.
