For many breast cancer patients, the road to recovery may present hidden complications related to breast reconstruction following a mastectomy. The insertion of foreign materials such as silicone breast implants can lead to implant malposition, a condition that affects a significant number of patients even years after surgery.
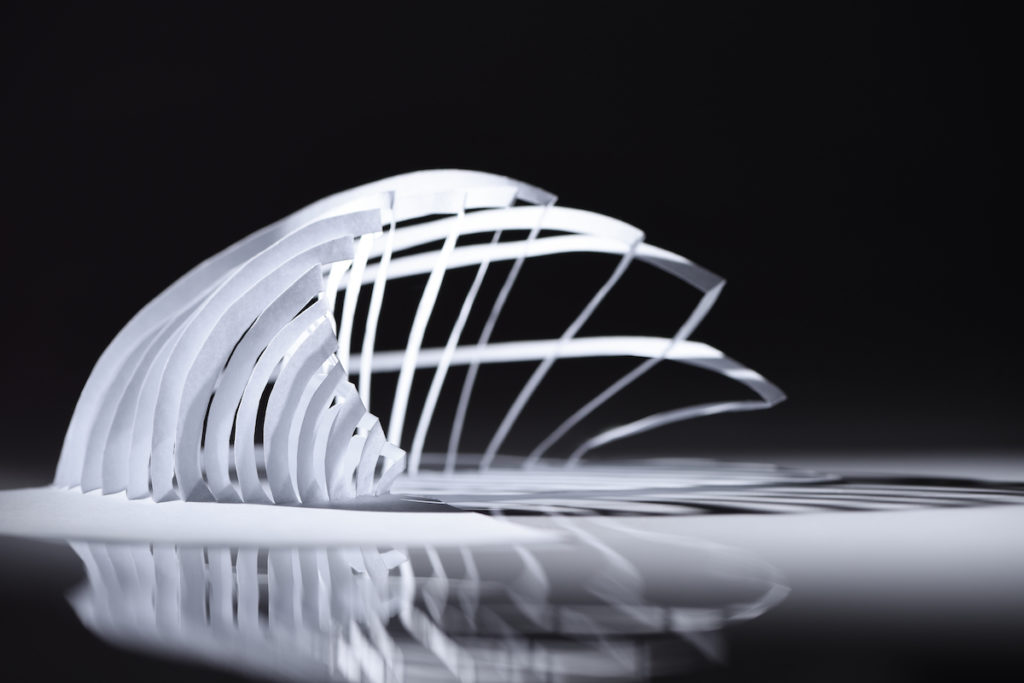
Now, researchers from the University of Pennsylvania have used the principles of a papercutting technique known as kirigami to safely and more securely cover implants while also using less material. The research, published in Advanced Materials, led by Shu Yang in the School of Engineering and Applied Science, describes how leveraging kirigami design practices and computational modelling offers enhanced flexibility and expandability to provide surgeons with an easier-to-use stretchable material that can better wrap around implants, thereby reducing the risk of malpositioning.
“We’ve taken the materials that currently use in operation rooms for breast reconstruction and addressed two of its major pitfalls by using kirigami designs,” says Yang, senior author of the paper. “Our technique allows the reconstructed breast to more securely take on a more natural shape and can substantially reduce the costs associated with these surgeries.”
Following a series of discussions with Suhail Kanchwala, a plastic surgeon and professor of surgery in the Perelman School of Medicine, the researchers began examining new possibilities for current breast implant wrapping material, called acellular dermal matrices (ADMs). These are a type of surgical mesh that are usually derived from human or animal skin. The cells are removed but the support networks—structural proteins like collagen, along with other extracellular matrix components—stay in place to facilitate the recovery of local blood supply and skin cell regeneration. Owing to their absence of cells and abundance of scaffolding-like elements, ADMs have gained popularity for their ability to minimize the reaction the immune system has to foreign objects and offer better support to implants.
The researchers suspected that ADM sheets could be altered in a unique way to address a concern with contemporary breast implants.
“An issue in breast reconstruction is that the manufactured implants are round, which doesn’t effectively mimic the more teardrop-like shape of natural breasts,” says Kanchwala. “So, our project wanted to figure out a way to put round implants under the ADM sheets in a way that allows the reconstructed breast to take on a more natural teardrop-like shape.”
Additionally, ADM sheets in their current configurations cannot conformably wrap around implants, as they do not preserve the curves and angles without forming wrinkles or voids. These can make the implant prone to rotating out of place and lead to mispositioning mishaps. Manufacturers’ response to these limitations has included introducing circular hole patterns to the ADM sheets or cutting out certain areas followed by stitching to cover more surface area effectively.
This story is by Nathi Magubane. Read more about ‘Kirigami Breast Reconstruction‘ at Penn Today.
