Immune system function in the microgravity of space
There are exciting plans to push the frontiers of human space exploration, sending astronauts deeper into the solar system than ever before. But before achieving a better understanding of the mysteries of the universe, crucial mysteries about how the human body responds to space environments need to be investigated.
Researchers Dan Huh, a bioengineer in the School of Engineering and Applied Science, and G. Scott Worthen, a professor of pediatrics in the Perelman School of Medicine and a physician-scientist in neonatology at Children’s Hospital of Philadelphia, are developing a technology to better understand how microgravity — an environmental condition in which people and objects appear to be weightless — negatively affects immune system function.
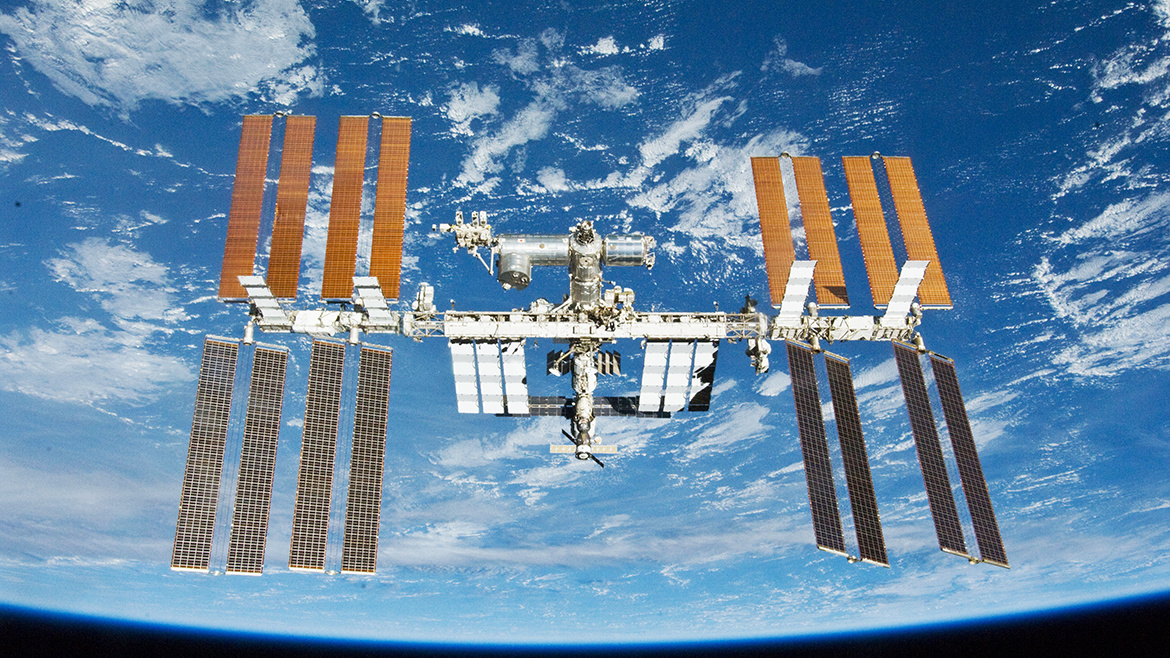
Understanding this occurrence is particularly important in microgravity environments such as those in a spacecraft and the International Space Station (ISS), where pathogens such as viruses, bacteria, and fungi are known to be present.
Huh and Worthen were recently awarded a $2 million grant co-sponsored by NASA, the Center for the Advancement of Science in Space, and the National Center for Advancing Translational Sciences at the National Institutes of Health. The funds will allow the researchers to engineer microphysiological systems, better known as “tissues-on-a-chip,” that model the human airway and bone marrow. Eventually, they hope to combine the models to emulate and understand the integrated immune responses of the human respiratory system in microgravity.
These chips will be launched to the International Space Station aboard a SpaceX rocket — once in 2019 and again in 2021 — to allow the researchers to see how the tissues respond to infections in the microgravity environment.
Huh has been working on this “tissue-on-a-chip” technology since it was first pioneered at Harvard. He and his team designed a microfluidic device in which they cultured lung and capillary cells on either side of a porous membrane and stretched them to mimic breathing in the lung.
For the space program, called “chips in space,” a team led by Huh and Worthen aims to model a condition called immunosuppression by developing an airway on a chip, sending it to the ISS and then infecting the airway tissue in microgravity to monitor what happens.
“It’s been known since the early days of human space flight that astronauts and cosmonauts become more prone to infection during or right after space flight,” Huh says. “Studies have shown that the microgravity environment in space can alter various aspects of immune function in the human body. For example, the number and activity of immune cells have been shown to decrease in microgravity. This unique environment can also change the production of cytokines and the expression of genes and surface receptors that play a critical role in immune responses. Much remains to be learned about the underlying mechanisms of these undesirable changes.”
Continue reading at Penn Current.
