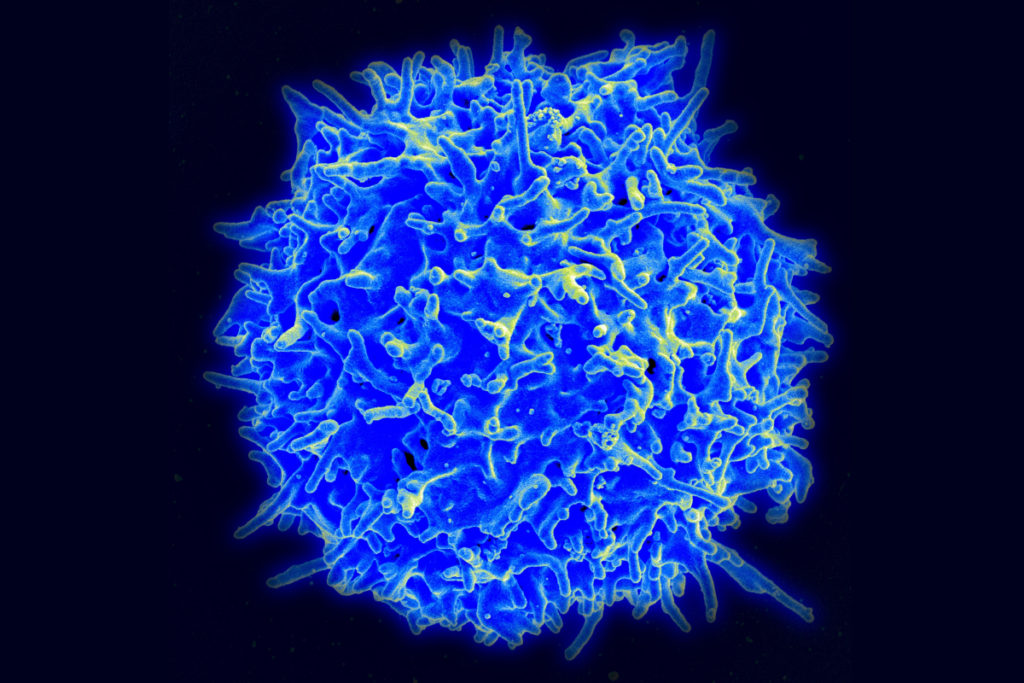
Our bodies are equipped with specialized white blood cells that protect us from foreign invaders, such as viruses and bacteria. These T cells identify threats using antigen receptors, proteins expressed on the surface of individual T cells that recognize specific amino acid sequences found in or on those invaders. Once a T cell’s antigen receptors bind to the corresponding antigen, it can directly kill infected cells or call for backup from the rest of the immune system.
We have hundreds of billions of T cells, each with unique receptors that recognize unique antigens, so profiling this T cell antigen specificity is essential in our understanding of the immune response. It is especially critical in developing targeted immunotherapies, which equip T cells with custom antigen receptors that recognize threats they would otherwise miss, such as the body’s own mutated cancer cells.

Jenny Jiang, Peter and Geri Skirkanich Associate Professor of Innovation in Bioengineering, along with lab members and colleagues at the University of Texas, Austin, recently published a study in Nature Immunology that describes their technology, which simultaneously provides information in four dimensions of T cell profiling. Ke-Yue Ma and Yu-Wan Guo, a former post doc and current graduate student in Jiang’s Penn Engineering lab, respectively, also contributed to this study.
This technology, called TetTCR-SeqHD, is the first to provide such detailed information about single T cells in a high-throughput manner, opening doors for personalized immune diagnostics and immunotherapy development.
There are many pieces of information needed to comprehensively understand the immune response of T cells, and gathering all of these measurements simultaneously has been a challenge in the field. Comprehensive profiling of T cells includes sequencing the antigen receptors, understanding how specific those receptors are in their recognition of invading antigens, and understanding T cell gene and protein expression. Current technologies only screen for one or two of these dimensions due to various constraints.
“Current technologies that measure T cell immune response all have limitations,” says Jiang. “Those that use cultured or engineered T cells cannot tell us about their original phenotype, because once you take a cell out of the body to culture, its gene and protein expression will change. The technologies that address T cell and antigen sequencing with mass spectrometry damage genetic information of the sample. And current technologies that do provide information on antigen specificity use a very expensive binding ligand that can cost more than a thousand dollars per antigen, so it is not feasible if we want to look at hundreds of antigens. There is clearly room for advancement here.”
The TetTCR-SeqHD technology combines Jiang’s previously developed T cell receptor sequencing tool, TetTCR-Seq, described in a Nature Biotechnology paper published in 2018, with the new ability of characterizing both gene and protein expression.
“The gene and protein expression of T cells is important because they tell us how activated T cells are, or their lack of activation, which occurs in the case of cancer or prolonged infection,” says Jiang. “This can help us to identify biomarkers that can be used to modulate T cell function in diseases.”
To validate TetTCR-SeqHD, the team chose CD8+ T cells, a variety that contribute to adaptive immunity, and found that the tool was able to sequence receptors on those T cells with 98 percent precision. By exposing those T cells to a panel of antigens derived from the flu virus and the Epstein-Barr virus, the team was then able to characterize their antigen specificity, cell subtypes, or activation status, and T cell proliferation status.
Then using this technology, the team decided to profile antigens related to Type 1 diabetes, as the disease is an autoimmune disorder in which T cells kill insulin-producing cells.
“We profiled a panel of 209 Type 1 diabetes-related antigens in a cohort of eight Type 1 diabetes patients and 10 healthy individuals,” says Jiang. “And we discovered three antigens in that panel whose binding T cell frequencies are higher in Type 1 diabetes patients compared to that in healthy controls. In addition, we found a T cell receptor that responds to both diabetes and microbiome antigens, potentially supporting the link between the gut and immune system.”
The discovery of this cross-reactivity of these particular antigens and the T cell receptor led to another new ability of this technology.
“Because we are able to generate high-throughput data on tens of thousands of single T cells interacting with hundreds of antigens using this method, we can look at multiple antigen binding profiles simultaneously and predict putative cross-reactions in antigens and T cells,” says Jiang. “This can then open doors to see where systems, diseases, cancer and immunotherapies connect. In fact, some of our next research will investigate putative cross-reactions between neurodegenerative diseases and the immune system.”
This new method of profiling T cells and their antigen specificity is not only useful in researching the fundamentals of T cell function, it can be used to develop better targeted immune therapies, an overarching goal of Jiang’s work.
“Each person has a huge safety net of T cells that respond to invaders in the body, even if the body has never encountered that particular antigen,” says Jiang. “This technology can help us understand why some people fight off infections while others get sick. It can show us which T cell receptors are good candidates for therapeutics and where our T cell communities may have weak spots.
“We can take advantage of our T cells’ ability to adapt as well as their ability to learn and remember specific invaders through vaccination,” she says. “Our body is constantly learning and adapting to the environment, and we now have a powerful tool to help us make these connections.”
