From COVID vaccines to cancer immunotherapies to the potential for correcting developmental disorders in utero, mRNA-based approaches are a promising tool in the fight against a wide range of diseases. These treatments all depend on providing a patient’s cells with genetic instructions for custom proteins and other small molecules, meaning that getting those instructions inside the target cells is of critical importance.
The current delivery method of choice uses lipid nanoparticles (LNPs). Thanks to surfaces customized with binding and signaling molecules, they encapsulate mRNA sequences and
smuggle them through the cell membrane. But with a practically unlimited number of variables in the makeup of those surfaces and molecules, figuring out how to design the most effective LNP is a fundamental challenge.
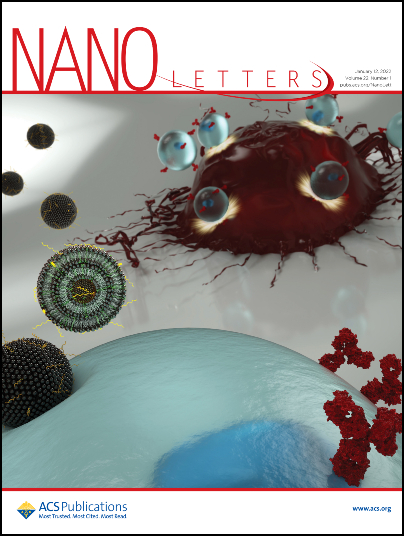
Now, in a study featured on the cover of the journal Nano Letters, researchers from the University of Pennsylvania’s School of Engineering and Applied Science and Perelman School of Medicine have now shown how to computationally optimize the design of these delivery vehicles.
Using an established methodology for comparing a wide range of variables known as “orthogonal design of experiments,” the researchers simultaneously tested 256 candidate LNPs. They found the frontrunner was three times better at delivering mRNA sequences into T cells than the current standard LNP formulation for mRNA delivery.
The study was led by Michael Mitchell, Skirkanich Assistant Professor of Innovation in the Department of Bioengineering in Penn’s School of Engineering and Applied Science, and Margaret Billingsley, a graduate student in his lab.
They collaborated with one of the pioneers of CAR T therapy, Carl June, Richard W. Vague Professor in Immunotherapy and director of both the Center for Cellular Immunotherapies in the Abramson Cancer Center and the Parker Institute for Cancer Immunotherapy at Penn’s Perelman School of Medicine, as well as with the Center’s Director of Research Technologies and Innovation, Neil Sheppard, Adjunct Associate Professor of Pathology & Laboratory Medicine.
“Orthogonal design of experiments is an established method of optimizing nanoparticle platforms for other applications, but this is the first time we’ve applied it to the development of LNPs for immune-cell-specific applications,” says Billingsley. “Because this method is established as an efficient means to screen a large library of LNPs using only a minimal number of representative formulations, it allows for the more high-throughput development of LNPs for delivery to immune cells.”
The study is a follow-up to an earlier Nano Letters paper, in which the researchers showed that mRNA-carrying LNPs were a more effective way of genetically modifying the T cells used in cancer immunotherapy.
“This study shows how potent LNPs can be designed more rapidly for use in the immune cell space,” says Mitchell, “but it also shows that we can potentially use this method to further optimize LNPs for other mRNA therapeutic applications.”
Alex Hamilton, Savan Patel and Kelsey Swingle, members of the Mitchell Lab, and David Mai, member of the June Lab, also contributed to this study.
The research was supported by a Burroughs Wellcome Fund Career Award at the Scientific Interface, a National Institutes of Health (NIH) Director’s New Innovator Award (DP2 TR002776), grants from the American Cancer Society (129784-IRG-16-188-38-IRG), and the National Institutes of Health (NCI R01 CA241661, NCI R37 CA244911, and NIDDK R01 DK123049), a Tau Beta Pi Graduate Research Fellowship, the NIH Training in HIV Pathogenesis T32 Program (T32 AI007632), and National Science Foundation Graduate Research Fellowships (Award 1845298).
